Congenital Atresia of the Nasolacrimal Duct
A 3-month-old infant was referred to a local ophthalmologist after her parents noticed epiphora and recurrent infections next to her eyes. Recognizing the symptoms of blocked nasolacrimal ducts, the ophthalmologist dilated the child’s eyes to flush out the ducts. Still, the infections persisted, so the patient was referred to the Duke Eye Center.
After examining the patient, Duke pediatric ophthalmologist Laura Enyedi, MD, reached out to Eileen Raynor, MD, pediatric head and neck surgeon at Duke, to perform nasolacrimal duct intubation to clear out the ducts.
Together, Enyedi and Raynor dilated the infant’s nasolacrimal duct with a probe so they could pass a tube down into the nose to allow the area to drain. Yet, on both sides, the probe ran into bone. The nasolacrimal duct appeared to be obstructed by a bony blockage.
Question: What procedure did Raynor and Enyedi perform to clear the obstruction?
Answer: Raynor and Enyedi performed endoscopic dacryocystorhinostomy to create a new opening for the nasolacrimal duct (Figures 1–3). Her recurrent infections were almost immediately resolved.
After the first surgery was unsuccessful, findings on computed tomography confirmed that the patient’s nasolacrimal ducts “dead-ended” into the maxilla, leading to a backup of fluid that provided the ideal environment for the growth of microorganisms.
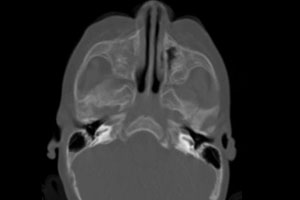 FIGURE 1. Computed tomography after dacryocystorhinostomy |
Raynor notes that this case was highly unusual. “You will sometimes see some blockage due to a little cyst or something like that,” she says. “But I’ve never seen a case where the nasolacrimal ducts don’t form at the end on both sides or at such a young age.”
To modify the procedure for an infant, Raynor and Enyedi used small instrumentation and employed the optical tracking system Brainlab (Munich, Germany), which allowed them to confirm their location in the patient’s nose as they performed surgery.
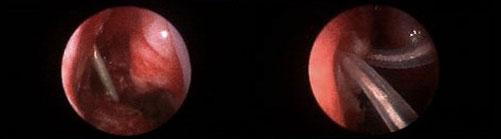 FIGURE 2. Right lacrimal duct opening before (left) and after (right) dacryocystorhinostomy |
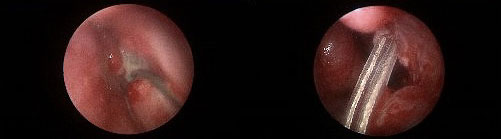 FIGURE 3. Left lacrimal duct opening before (left) and after (right) dacryocystorhinostomy |
Raynor reports that the surgery went well. Working in conjunction with other specialties, such as plastic surgery, pediatric pulmonology, gastroenterology, and, in this case, ophthalmology, she says, allows her to offer complex surgeries and provide care to a broad range of patients.
“My goal is also to minimize anesthesia exposures, if possible,” she adds. “There aren’t a lot of great data about the long-term effects of anesthesia over time. So, I think that the more things can be done in a combined manner, the better it is for the patient.”