HIFU Improves Outcomes in Select Patients With Prostate Cancer
High-intensity focused ultrasonography (HIFU) provides a new alternative for controlling cancer and preserving urinary and sexual function in patients with prostate cancer and offers a fast recovery time. However, the technique is performed by very few hospitals.
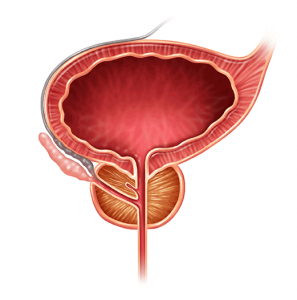
Ideal candidates for HIFU are aged 55 to 75 years and have intermediate-risk cancer. They should have a small-sized prostate gland (≤ 40 cc in size; 25 cc is preferable) and no disease beyond the prostate and localized tumors, says Cary Robertson, MD, a urologic oncologist at Duke.
Robertson was the principal investigator of a national clinical trial that compared the effectiveness of HIFU with cryotherapy as an initial treatment option for men with newly diagnosed, low-grade prostate cancer.
Of the 135 patients enrolled in the trial, 27 were treated with the Ablatherm HIFU device (EDAP TMS, Vaulx-en-Velin, France) at Duke. Safety mechanisms included a shutdown of the device if the heat generated during HIFU came too close to the rectal wall. Movement detectors also monitored any positional change.
Robertson says that treating the entire gland with HIFU can target cancer that may be missed on biopsy. The device is designed to robotically sweep back and forth across the entire gland following the planning that precedes treatment. The shrinkage of prostate tissue is notable after treatment, averaging a 5-cc prostate volume following HIFU.
Study patients undergoing whole-gland coverage experienced a urinary leakage rate of 2% after the treatment. The whole-gland treatment was then followed by recovery of baseline erections sufficient for intercourse in 25% of men, with 25% experiencing significant partial recovery of function. These outcomes are similar to reported surgical outcomes for radical prostatectomy.
HIFU doesn’t spare the urethra (which passes through the gland); thus, following treatment, the entire gland can swell and close. “Patients are managed with a urinary catheter for awhile after treatment,” Robertson explains. Those with more-enlarged glands may need to have their glands trimmed prior to HIFU because of potential swelling difficulties.
The procedure requires anesthesia, although patients are discharged the same day, typically with a catheter that remains in place for 1 to 2 weeks.
Typically, the heat treatment isn’t painful, but it may negatively affect the nerves at the bladder base. Patients may feel a sense of urgency or spasm during the first 24 hours. However, most patients don’t require narcotics, Robertson says.
“In the future, we may be more comfortable treating just part of the prostate,” Robertson says. “Duke Urology sponsors an annual symposium on focal therapy of urologic tumors, and it is very timely that HIFU is now approved for treatment of prostate tissue. HIFU is an ideal technology for focal prostate therapy.”
If only a portion of the gland is treated, as many as 80% of patients may remain sexually functional, with minimal impact on urinary control, which has been seen with previous international studies.
Duke Urology provides many other men’s health services, including the diagnosis and treatment of urologic cancers, male wellness, urologic reconstructive procedures, and penile implants, to help improve quality of life and manage the survivorship phase after treatment. To refer a patient, call 844-790-2013.