Middle-Aged Man Develops OSSN After Years of Sun Exposure

FIGURE 1. Patient's eye with a spot suspicious for ocular surface squamous neoplasia
A 62-year-old white man with a long history of sun exposure was referred to the Duke Eye Center after his ophthalmologist detected a spot on his left eye during routine observation. At Duke, ophthalmologist Gargi Vora, MD, examined the patient and determined that the spot was suspicious for ocular surface squamous neoplasia (OSSN; Figure 1).
Question: What noninvasive approaches did Vora employ to confirm the diagnosis and treat the OSSN?
Answer: Vora performed a detailed slit-lamp examination with rose bengal staining of the ocular surface, anterior segment optical coherence tomography (OCT; Figure 2), and incisional biopsy to confirm the OSSN diagnosis. She successfully treated the patient with topical chemotherapy.
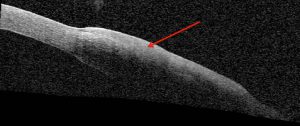
FIGURE 2. Anterior segment optical coherence tomography reveals a thickened, hyper-reflective epithelium (red arrow)
After examining the patient’s eye on initial presentation, Vora was already concerned the patient had OSSN, but anterior segment OCT helped her confirm the diagnosis without resorting to surgery. “Anterior segment OCT allows you to do a high-resolution, cross-sectional analysis of the epithelium that can help make the diagnosis of OSSN and help determine whether the tumor is invasive,” she says.
Anterior segment OCT of the patient’s left eye revealed a thickened, hyper-reflective epithelium with an abrupt transition between normal and abnormal epithelium—characteristic of OSSN. Vora confirmed the diagnosis by performing incisional biopsy at the slit-lamp.
Rather than resecting the lesion, Vora prescribed the patient a 4-month course of topical interferon α-2b eye drops. She explains that, for certain cases, she sometimes goes directly to surgery, but more often she prefers to try topical chemotherapy first. If the drops aren’t effective, then she can still take the patient to surgery.
At the patient’s 8-week follow-up appointment, halfway through his treatment, the mass had almost resolved. However, he still had some injection and surface irregularity on his eye, suggesting that some microscopic cells of the tumor remained. Vora recommended continuing with the treatment for the remaining 2 months and then reassessing the patient's condition.

FIGURE 3. Patient's eye following 4 months of topical chemotherapy
By the end of the 4-month course of topical chemotherapy, the patient’s eye looked white and quiet, without evidence of a lesion (Figure 3). Anterior segment OCT confirmed a normal epithelium. Vora says she will continue to monitor the patient every 4 months for the first year, every 6 months for the second, and then yearly thereafter. Given his history of sun exposure, she explains, he will need to have both eyes routinely examined for the rest of his life.
“If I had seen this patient 10 years ago, we would have said, 'Let’s take you to surgery and find out what it is,'” Vora remarks. “But now we can use anterior segment OCT to help us make a diagnosis. That helped us avoid the operating room, which can be expensive and is not completely risk-free. It can be quite an invasive surgery, and rehabilitation for the patient can take a long time. These drops are actually very effective and have minimal adverse effects.”