Multi-Dimensional Models Take Personalized Medicine a Step Further
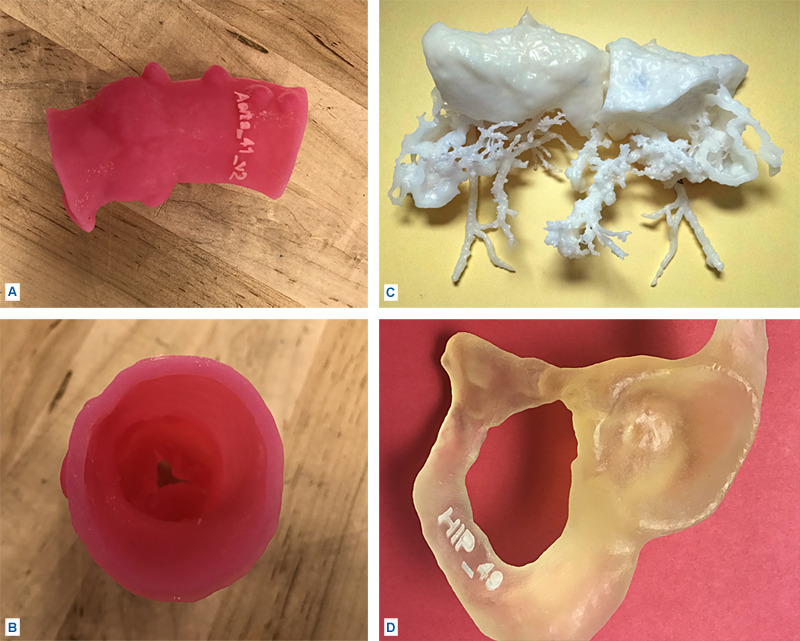 FIGURE: (A) aortic valve, (B) aortic valve, top view, (C) organs of conjoined twins, (D) hip joint.
FIGURE: (A) aortic valve, (B) aortic valve, top view, (C) organs of conjoined twins, (D) hip joint.
A fast-growing laboratory at Duke is serving multiple specialties with sophisticated software technology that evaluates data from an image produced with any imaging modality and creates multi-dimensional (multi-D), virtual models of patients’ anatomical structures, which are then printed in Duke’s Innovation Co-Lab.
Studying 3-dimensional (3-D) models of anatomical structures enables clinicians to examine the structures from different angles, plan courses of treatment, simulate surgical procedures, and demonstrate procedures to patients.
The Multi-Dimensional Image Processing Lab (Multi-D Lab) at Duke Radiology is at the center of the entire process. “Any time a provider has a question that could be answered from studying a model or is thinking about how best to perform a complex procedure, the discussion starts in the lab to determine feasibility,” says Daniele Marin, MD, medical director of the Multi-D Lab.
Marin notes that part of the lab’s role is to facilitate discussion and gather input from different departments such as radiology and engineering, ensuring that the best materials are used, that the printing process is optimized, and that the provider works closely with the engineer responsible for printing the file to ensure the model is clinically accurate. “This multidisciplinary, collaborative approach makes the entire process more impactful and is a unique advantage we have at Duke,” he says.
The technology used for modeling is so advanced that the structures can be very complex, such as an aortic valve, a brain with ventricles, an organ requiring transplant, a congenital abnormality in a newborn, or any other complex case (see Figure).
Susan A. Whitney BSRT(R)(N)(CT), supervisor of the Multi-D Lab, explains that the modeling process relies on a team of highly qualified individuals with advanced certifications in radiology who understand the images and the goal of the 3-D printed models and who are able to use the software to produce the intricate models.
“The team creates a structure in multiple parts, such as the hollow aorta, the leaflets, and the calcium on an aortic valve, with supports resembling a roller-coaster track to build up the model,” Whitney says. “After printing, our refinement team removes the support structure in a painstaking process that can take more than 4 hours, and then the model undergoes a strict quality control process to ensure it’s clinically accurate.”
As part of the quality control process, technologists superimpose a contour of the printable file on the patient’s original imaging anatomy to ensure the model is clinically correct prior to printing. The file undergoes an analysis using advanced software to ensure the structural integrity of the model and to allow any defects to be corrected. The 3-D printed model undergoes a surface scan to determine accuracy and is then reviewed by a radiologist to verify its correctness.
To learn more about the services provided at the Multi-D Lab, including upcoming 3-D printing workshops, or to discuss the feasibility of creating a model, contact the lab at 919-668-6337 or email susan.churchill@duke.edu.
“There is quality assurance at every step, from image acquisition to segmentation, to comparing the printable file to the patient’s original data, to confirming the accuracy of the print, and to making sure no structures were accidentally removed during the refinement process,” says Whitney.
Sreekanth Vemulapalli, MD, a Duke cardiologist, is directing a research project studying the blinded cases of 20 Duke patients who underwent transcatheter aortic valve replacement (TAVR) insertions before anatomical models were available. “Leak assessments can be attempted with the use of CT scanning technology to simulate the insertion of the device into the aorta,” he says. “But it’s obviously more intuitive and powerful to physically replicate the procedure. And 3-D printing appears to be the perfect response to this clinical problem.”
Researchers use post-insertion ultrasounds for the leak studies and then review the device and its profile as well as the patient’s leak history. The goal is to achieve quantitative assessments. “It’s not good enough to say, yes, we see a leak,” says Vemulapalli. “We want more data and we are using the models to help us. How big is the leak and exactly where is it on the aortic valve?”
In the future, Marin anticipates that the Multi-D Lab will soon be at the forefront of moving beyond printing only hard surfaces to using flexible materials that simulate soft tissue, leading to new possibilities for demonstrating pathologies and further tailoring medical treatment to an individual’s needs.