OCT May Have Potential as Alternative to MRI for Measuring Posterior Eye Shape
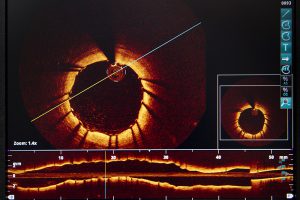 A study published by Duke and Duke-NUS investigators in the July 2016 issue of Investigative Ophthalmology & Visual Science demonstrates the potential of using commercially available optical coherence tomography (OCT) as an alternative to magnetic resonance imaging (MRI) to measure posterior eye shape, an important indicator in studying the development of myopia.
A study published by Duke and Duke-NUS investigators in the July 2016 issue of Investigative Ophthalmology & Visual Science demonstrates the potential of using commercially available optical coherence tomography (OCT) as an alternative to magnetic resonance imaging (MRI) to measure posterior eye shape, an important indicator in studying the development of myopia.
The study comes as part of ongoing efforts at Duke to develop OCT as a practical alternative to MRI for measuring posterior eye shape to facilitate the early detection of high myopia and pathologic myopia.
“There are different classification methods for eye shape, but the bottom line is they all require performing MRI of the eye,” says Anthony Kuo, MD, lead author on the study. “But MRI is expensive, and it’s not the easiest thing to obtain, so we thought, 'We have OCT, which is a 3-dimensional eye scanner. Can it give us the same sort of information?'”
The results from this initial study suggest the answer may be yes. When Kuo and his team compared posterior eye measurements derived from distortion-corrected OCT with those generated from MRI, they found that 2 important measures of posterior eye shape—asphericity and sphericity—were roughly the same. Imaging was obtained from OCT and MRI previously acquired as part of 2 epidemiologic studies conducted in Singapore at Duke-NUS.
Kuo admits that he was surprised by the results: “The commercially available OCT used in the study only generates images of a small area of the back of the eye. We didn’t expect it to work this well.”
Still, he stresses that the current commercially available version of OCT is not capable of replicating MRI on an individual level. Rather, data taken from OCT in the study successfully replicated the same overall trend in the population revealed by the MRI data: The more myopic patients are, the more oval-shaped their eyes tend to be.
In the future, Kuo hopes to develop OCT capable of scanning nearly the entire eye. “If we can measure posterior eye shape based on just a small part of the eye, a more complete 3-dimensional model of the eye should allow us to reproduce what MRI does and with a lot better resolution,” he says. “Our long-term hope is to be able to see young patients, scan their eyes, and, based on the data, determine whether their nearsightedness is at high risk of becoming pathologic down the road and in need of intervention now.”
Although use of OCT for whole-eye imaging in the clinic is probably many years away, he adds that Duke is playing an important role in laying the groundwork.
“We want to continue to push eye imaging forward and help define the next generation of imaging devices to change and improve eye care,” Kuo concludes.
