Personalizing Options for Vaginal Repair
A married, 65-year-old woman with 2 adult children called her primary care physician because she noticed a concerning bulge near the opening of her vagina. At a Duke Primary Care clinic, she described something bulging from her vagina that seemed to grow in size after straining to have a bowel movement on a day she had gardened for hours.
Question: What was causing the bulge, and how was the patient treated?
The physician referred the patient to Duke Urogynecology for evaluation of pelvic organ prolapse. The patient said she now had to push the bulge inside every day. An otherwise healthy, active woman, she was not experiencing pain but felt incomplete bladder emptying and hesitancy when voiding.
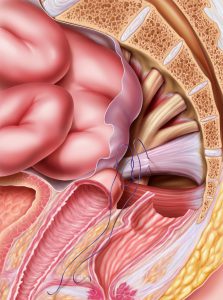
Amie Kawasaki, MD, the treating urogynecologist at Duke, discovered that the patient's anterior vaginal wall supporting her bladder as well as the uterus had prolapsed beyond the opening of her vagina. After measurements, the patient was diagnosed with stage 3 uterovaginal and anterior vaginal prolapse. Several nonsurgical and surgical treatment options were discussed.
“Some prolapse is very mild and can be observed and treated with physical therapy, but more significant prolapse can either be managed with a silicone pessary or with surgery,” Kawasaki says.
Prolapse can be surgically corrected with vaginal, minimally invasive (laparoscopic, robotic-assisted, or both methods), or abdominal surgery. Some surgical procedures are performed with native tissue, whereas others incorporate synthetic mesh material.
Aware of all the options, the patient desired the longest-lasting repair so that she could resume gardening and other activities for years to come. The urogynecologist performed robotic-assisted laparoscopic hysterectomy with mesh sacrocolpopexy. The indication for this procedure is advanced vaginal prolapse involving the uterus or vaginal vault in the case of prior hysterectomy.
Postoperatively, the patient was comfortable and ate a regular dinner in the hospital. Six weeks later, she returned to all of her typical activities.