Simultaneous Occlusion of the Carotid and Middle Cerebral Arteries
 A 79-year-old man experiencing total paralysis on his right side was rushed to his local community hospital. Upon his arrival at Nash General Hospital, emergency medicine physicians confirmed that the patient was having a major stroke.
A 79-year-old man experiencing total paralysis on his right side was rushed to his local community hospital. Upon his arrival at Nash General Hospital, emergency medicine physicians confirmed that the patient was having a major stroke.
However, the hospital did not have the resources to treat a patient with such a large stroke, and the nearest comprehensive stroke center at Duke University Hospital was more than 1 hour away.
Question: What did the emergency medicine physicians do to ensure the patient was treated as soon as possible, and how was he treated?
Answer: Nash General Hospital is an affiliate of the Duke Telestroke Network, so the emergency medicine physicians on staff were able to consult neurocritical care specialists at Duke Health. The patient was initially treated with tissue plasminogen activator (tPA) prior to his transfer to Duke Health for mechanical thrombectomy.
Prior to obtaining computed tomography (CT), the emergency medicine physicians at Nash activated a stroke code, which initiated a telestroke consult with the neurologist on call at Duke. As soon as CT had been performed, the neurologist at Duke tele-examined the patient.
Carmelo Graffagnino, MD, medical director of the Duke Comprehensive Stroke Center, explains, “Because we don’t have our hands and feet in the room, the nurses become our surrogates, and the camera becomes our eyes. The nurses have learned exactly what we’re looking for when examining a patient, so they’ve really become our partners.”
Findings on CT indicated that the left carotid artery was occluded, so the emergency medicine physicians administered tPA to help dissolve the clot. The patient was then transported to Duke University Hospital.
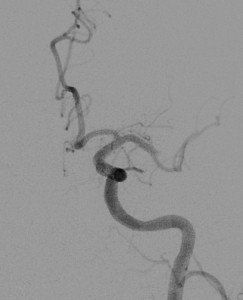
At Duke, results on CT angiogram confirmed the left carotid occlusion and further revealed that the patient’s middle cerebral artery was totally occluded, indicating that a large area of the dominant hemisphere was cut off from its blood supply. The neurosurgical team was contacted, and the patient was sent to the catheterization suite.
Fernando Gonzalez, MD, performed mechanical thrombectomy using a stent retriever to remove both clots (Figure), and then the patient was admitted to intensive care.
“Whereas 2 years ago we did 6 or 7 thrombectomies, last year we performed 76,” says Gonzalez. “People are recognizing that it’s a safe procedure that really works.”
New Stroke Guidelines Recommend Mechanical Thrombectomy
In 2015, the American Heart Association/American Stroke Association issued guidelines for treating patients following stroke who have clots in large arteries of the brain. Although tPA should still be administered to these patients as soon as possible, if tPA is unable to fully dissolve the clot, then mechanical thrombectomy should be performed within 6 hours of stroke onset. Carmelo Graffagnino, MD, medical director of the Duke Comprehensive Stroke Center, says Duke’s telemedicine model aligns well with the new guidelines. Community hospital staff can administer tPA, and, with the support of Duke neurologists, quickly identify patients requiring transfer for mechanical thrombectomy. Fernando Gonzalez, MD, a Duke neurosurgeon, stresses the importance of exploiting the integrated model for early treatment: “Time is brain.”
When the patient’s condition was stable a few days later, he was transferred to the care of the stroke team, who helps rehabilitate patients following stroke and investigates the potential cause of the stroke.
In this case, Graffagnino noticed the patient’s glycated hemoglobin levels were borderline diabetic, so he began to monitor the patient’s blood sugar levels and to educate him on diet and exercise. He also discovered the patient had atrial fibrillation and prescribed blood thinners, thus decreasing the patient's risk of repeat stroke from approximately 8% to less than 1%.
One week after being admitted, the patient had almost completely recovered. At a 90-day follow-up visit, Graffagnino reports that the patient’s cholesterol, blood pressure, and heart rate were controlled, and his only sign of having had a major stroke was that he occasionally mixed up his words.
Gonzalez remarks, “The early recognition and treatment of stroke is the main contributor to our success. That depends on a large team of people—not just the neurosurgeons and neurologists at Duke but also emergency medical services, emergency medicine physicians, nurses, and technicians at the community hospital.”
Graffagnino agrees, adding, “It’s really an amazing example of a village. The electronic world lets us go to patients and, when necessary, bring them to us, but a village really starts in the community.”