What’s New in Hyperparathyroidism
Know the Disease
Use a mnemonic device to remember the end-organ consequences of hyperparathyroidism:
- Bones: Thinning of bones, osteoporosis
- Stones: Kidney stones
- Moans: Either from depression or anxiety
- Groans: Peptic disease pain
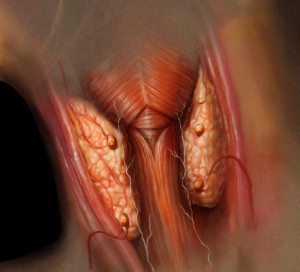
Primary hyperparathyroidism, which can lead to a high level of blood calcium, is a common disease that involves at least 1 of the 4 parathyroid glands. Commonly, the condition is due to a benign tumor in a single gland.
In women 65 to 74 years of age, the disease incidence is about 1 in 1,000 and increases with age. “Although mortality is not necessarily increased, significant morbidity is associated with the condition,” says Thomas Weber, MD, a metabolic bone disease and parathyroid expert at Duke.
When to Refer
Most patients with laboratory test results that indicate hyperparathyroidism may be asymptomatic. If calcium levels are high, then more frequent urination, increased thirst, confusion, forgetfulness, mental cloudiness, bone pain, and weight loss may be present.
Referral to endocrinologists when patients are asymptomatic or challenging to diagnose may be warranted.
Guidelines published in 2014 for asymptomatic primary hyperparathyroidism include recommendations for a more extensive evaluation of the skeletal and renal system to search for complications that may not be evident. In addition, they address new indications for surgical referral (eg, more extensive evaluation for kidney stones through abdominal radiography or ultrasonography).
The guidelines also specify approaches to monitoring patients who do not have a clear indication for parathyroid surgery.
Potential Emerging Concerns
Some groups in Europe have found that hyperparathyroidism is associated with higher rates of mortality and are pursuing further research, although patients living in Europe have traditionally presented with more significant hypercalcemia than their counterparts from the United States. Investigators are now examining whether hyperparathyroidism could lead to an increased risk of cardiovascular outcomes and stroke, possibly related to the accumulation of calcium in blood vessels.
A group from Columbia University was the first to identify a new potential patient phenotype called normocalcemic primary hyperparathyroidism, which is defined as an elevated parathyroid hormone level with a normal level of calcium.
“Studies show that these patients can experience bone loss and have a risk of kidney stones, so they may show signs of this disease even when calcium is not frankly elevated,” Weber says. To make a diagnosis of normocalcemic hyperparathyroidism, clinicians must rule out vitamin D deficiency and kidney dysfunction.
Advanced Care in Large Endocrine Programs
Large centers for endocrine care can offer more advanced and personalized treatments for patients with primary hyperparathyroidism. For example, Duke has an established and expanding program in minimally invasive parathyroidectomy that affords a more rapid recovery time for patients. To enhance the delivery of efficient and evidence-based care, Duke has created an algorithm in its electronic health record system that utilizes the recommendations from the 2014 guidelines.
Preoperative localization of parathyroid adenoma is also a critical aspect of patient care. At Duke, radiologist Jenny Hoang, MD, performs 4-dimensional computed tomography in real time to detect the locations of candidate lesions.
Duke also specializes in more complex treatments. If all 4 parathyroid glands are involved (typically due to a genetic mechanism), then clinicians carefully remove 3.5 glands, thus leaving one-half of a gland intact to avoid hypoparathyroidism. Weber notes that hypoparathyroidism is a potentially serious health condition that can be challenging to treat.